ONCO Fertility
Oncofertility is the medical discipline that merges oncology and reproductive endocrinology to enhance the fertility prospects of individuals with cancer and those who have overcome it. Ensuring fertility preservation is considered a basic right for everyone.
This field bridges the expertise of oncologists and reproductive endocrinologists to address the fertility challenges faced by young cancer patients at risk of losing ovarian or testicular function. Innovations in fertility preservation are creating new opportunities for individuals facing decreased fertility due to cancer. Cancer and its treatments may compromise one’s reproductive capabilities. While the responsibility of introducing fertility preservation options falls on the oncology team, the actual procedures to safeguard fertility are carried out by reproductive endocrinologists or fertility specialists.

Numerous factors contribute to why individuals diagnosed with cancer might not receive information about fertility preservation from their healthcare providers. Some common explanations provided by medical teams include concerns about the patient’s ability to afford the procedures, the belief that there isn’t enough time to implement such measures before treatment begins, or the perception that the patient is already overwhelmed and might not be able to cope with additional discussions on fertility amidst their emotional turmoil.
Types and Locations of Cancer
Cancers targeting the reproductive systems in both men and women, or the neuroendocrine system (including brain tumours or metastatic growths) can lead to infertility by causing direct damage. At the time of diagnosis, a patient’s fertility potential may already be diminished due to overall health degradation.
Chemotherapy Agents and Dosages
Alkylating agents carry a moderate to high risk of infertility. Platinum-based drugs, anthracyclines, and taxanes present a moderate infertility risk, whereas 6-mercaptopurine, methotrexate, 5-fluorouracil, vincristine, bleomycin, and actinomycin are associated with a low to negligible risk. High-dose chemotherapy, particularly when combined with hematopoietic stem cell transplantation, frequently results in severe and typically irreversible infertility.
Radiation Therapy
Total body irradiation and cranial-spinal irradiation significantly endanger the hypothalamic-pituitary-gonadal axis. For females, whole abdominal and pelvic radiation poses a high infertility risk, with specific dose thresholds based on age and developmental stage. The testes are extremely sensitive to radiation, with doses as low as 0.15 Gy reducing sperm production and doses above 0.5 Gy potentially leading to azoospermia. Some recovery from radiation-induced azoospermia is possible, but it depends on the dose received by the testes.
Surgical Interventions
Surgeries involving the reproductive organs, or the neuroendocrine system can impair fertility.
Effects of Combined Treatments
Employing chemotherapy in conjunction with other treatment approaches can additionally influence a patient’s overall reproductive risk.
Available Fertility Preservation Methods
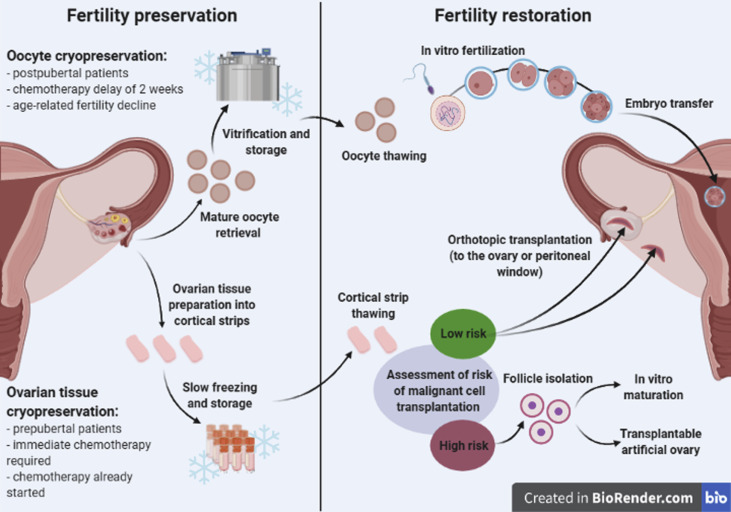
The choice of fertility preservation (FP) techniques varies based on the patient’s age, type of cancer, and the timeframe available before starting cancer treatment.
Fertility Preservation Techniques
Egg Freezing: This method involves cryopreserving a woman’s eggs for future use.
Embryo Freezing: Eggs are stimulated to mature through hormonal treatments, harvested, and fertilized with sperm to create embryos, which are then frozen. This procedure typically takes 2-6 weeks.
In Vitro Maturation (IVM): Immature eggs are collected without hormone stimulation and matured in a lab before or after freezing. This method is quicker, reducing delays in starting cancer treatment.
Sperm Freezing: Semen samples are collected and frozen for future use over several days.
Testicular Sperm Aspiration or Extraction: This minor surgical procedure retrieves sperm directly from the epididymis or testes for freezing, used when ejaculation does not produce sperm.
Tissue Banking: Ovarian or testicular tissue is removed and frozen for later transplantation to potentially produce eggs or sperm.
Reproductive Organ Shielding: Protecting the genital and pelvic areas with lead shielding during radiation treatment.
Ovarian Transposition: Surgically repositioning the ovaries outside the pelvic area to avoid radiation damage.
Gonadotropin-Releasing Hormone Agonists: Used to protect reproductive function during cancer treatment.
Summary
Oncofertility has grown from a concept into a well-established discipline backed by significant pre-clinical and clinical research. Advances in stimulation protocols, lab techniques, and cryopreservation have played a pivotal role in its success. The ongoing goal for researchers is to discover methods that not only preserve fertility but also maintain normal reproductive hormone levels for patients.
