In the journey toward parenthood, many factors come into play, and one that is increasingly recognized for its significant impact is Obesity. Defined as a disease characterized by excessive body fat that increases health risks, Obesity is clinically measured using the Body Mass Index (BMI). Understanding its effects and the available management strategies is crucial for optimizing reproductive outcomes for both men and women.
What is Obesity, and How is it Measured? BMI is calculated as weight in kilograms divided by height in meters squared (kg/m²). According to the World Health Organization (WHO) classification, a BMI of 30.0 kg/m² or higher is considered obese, with further classifications for Class I, II, and III Obesity.
It is essential to note that for South Asian populations, including those in India, lower BMI cutoffs (overweight ≥23.0 kg/m² and obesity ≥25.0 kg/m²) are often employed due to distinct body fat distributions and associated health risks.

A comprehensive initial assessment for Obesity in a reproductive medicine setting includes:
1. Clinical and Anthropometric Assessment: This involves documenting medical history, medication history, lifestyle factors (including nutrition and physical activity), and a physical examination to measure height, weight, body mass index (BMI), waist circumference (WC), and waist-to-hip ratio (WHR). WC and WHR are key for assessing central Obesity, a significant metabolic risk factor.
2. Laboratory Assessment: For patients diagnosed with Obesity, screening for metabolic comorbidities may include tests such as Fasting blood glucose,
Glycated Hemoglobin (HbA1c), Fasting lipid profile, Liver and renal function tests, Thyroid-Stimulating Hormone (TSH), and 25-hydroxyvitamin D levels.
The Profound Impact of Obesity on Reproduction
Obesity can significantly affect both female and male fertility.
For Women, the impacts include:
1. Ovulatory Dysfunction: There is a strong link between Obesity, menstrual irregularities and anovulatory infertility, often associated with Polycystic Ovary Syndrome (PCOS). Obese women can also have altered hormone levels even with regular cycles.
2. Reduced Natural Fertility: A higher BMI is directly associated with a longer time to conception.
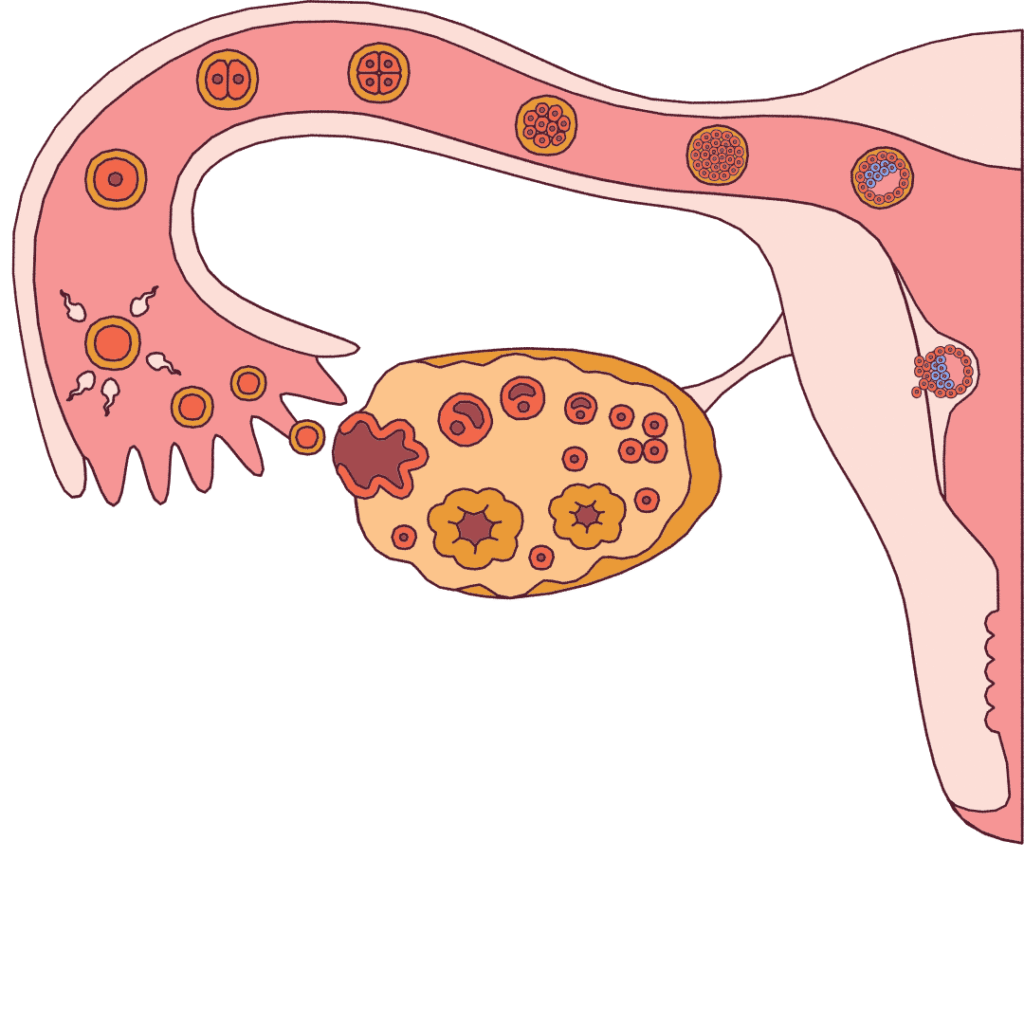
3. Assisted Reproductive Technology (ART) Outcomes: Women with Obesity typically require higher doses of gonadotropins for ovarian stimulation, resulting in fewer oocytes retrieved and lower implantation, clinical pregnancy, and live birth rates in IVF cycles.
4. Oocyte and Embryo Quality: Obesity can impair oocyte quality through mechanisms like mitochondrial dysfunction and increased oxidative stress.
5. Increased Miscarriage Risk: Obesity heightens the risk of miscarriage in both natural and assisted conceptions, even for euploid (chromosomally normal) pregnancies.
6. Pregnancy Complications: Maternal Obesity is a significant risk factor for conditions like gestational diabetes, hypertension, preeclampsia, and the need for a cesarean delivery.
For Men, Obesity can lead to:
1. Semen Quality Issues: It is associated with a higher incidence of low sperm count (oligozoospermia) and poor sperm motility (asthenozoospermia).
2. Hormonal Changes: Obesity can lead to lower testosterone levels and altered hormonal profiles, resulting from the conversion of androgens to estrogens in adipose tissue (fat).
3. Sperm Function Impairment: Observations include increased sperm DNA damage, mitochondrial dysfunction, and seminal oxidative stress.
A Tiered Approach to Weight Management for Fertility
A structured, tiered approach to weight management is recommended, starting with the least invasive methods.
1. First-Line: Lifestyle Modification This is the foundational step for all patients with Obesity seeking fertility treatment.
- Dietary Intervention: It involves recommending a daily calorie restriction of 500-600 kcal/day and encouraging a balanced diet with controlled portion sizes, reducing refined carbohydrates and fats. Referral to a nutritionist for a personalized diet plan is strongly recommended.
- Physical Activity: Engaging in at least 150 minutes of moderate-intensity aerobic activity per week (e.g., brisk walking) is essential.
- Behavioural Therapy: Cognitive Behavioral Therapy (CBT) can be beneficial, especially when integrated into a comprehensive lifestyle program, for achieving and sustaining weight loss.
2. Second-Line: Pharmacotherapy Medications may be considered for patients with a BMI ≥27 kg/m² and comorbidities or a BMI ≥30 kg/m² who have not achieved weight loss goals with lifestyle changes alone.
- Medication Options: These can include GLP-1 Receptor Agonists (e.g., Liraglutide, Semaglutide), which are effective for weight loss and may improve metabolic parameters and restore menstrual cycles in women with PCOS. Orlistat, a lipase inhibitor, and Phentermine/Topiramate, an appetite suppressant, are also options.
- Safety Note: Anti-obesity medications are contraindicated during pregnancy and must be discontinued prior to conception attempts. Patients should also be counselled on potential side effects.
3. Third-Line: Bariatric Surgery Referral to a bariatric surgeon is an option for women with a BMI ≥35 kg/m², with or without obesity-related comorbidities.
- Post-Surgery Conception: It is important to delay pregnancy for 12–18 months after bariatric surgery to avoid conception during rapid weight loss and potential nutritional deficiencies. A preconception nutritional status assessment is mandatory.
Special Considerations for ART: While Obesity significantly impacts live birth rates, it is crucial to remember that age-related decline in fertility has a greater impact, especially in older women. Therefore, the decision to delay ART for weight loss must be individualized, carefully balancing the benefits of weight reduction against the risks of declining ovarian reserve due to advancing age.
Conclusion: Managing Obesity in a reproductive medicine setting requires a standardized, evidence-based approach. By understanding the profound effects of Obesity on both male and female fertility and embracing tailored management plans—from lifestyle changes to medical interventions or, in some cases, surgery—patients can significantly optimize their chances of successful reproductive outcomes. Always consult with your healthcare provider to determine the best course of action for your circumstances.
