Challenges in Ovarian Stimulation: Insights from Dr. G.A. Rama Raju’s Lecture
Ovarian stimulation is at the heart of modern IVF treatment. While science has advanced dramatically over the past few decades—from natural cycles in the early days to today’s highly tailored stimulation protocols—the process still presents challenges. In a recent lecture, Dr. G.A. Rama Raju, Director of Krishna IVF Clinic, explored these challenges, highlighting both clinical realities and ongoing research.

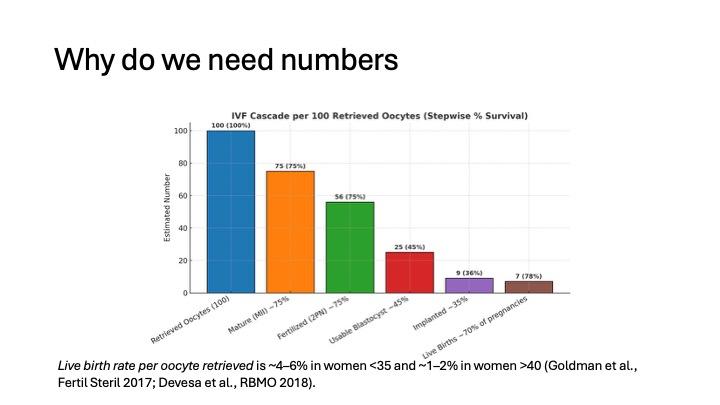
Why Numbers Matter in IVF
Success in IVF is not guaranteed with every egg retrieved. Research shows that the live birth rate per oocyte retrieved is only about 4–6% in women under 35 and drops to 1–2% in women over 40. This inefficiency underscores the importance of carefully balancing ovarian stimulation to retrieve enough eggs without compromising quality.
The Quality vs. Quantity Dilemma
Too few eggs: lower chance of pregnancy.
Too many eggs: potential health risks and compromised oocyte quality.
Oocyte Quality Concerns
Ovarian stimulation can sometimes negatively influence egg quality:
Pro-inflammatory changes in the follicular environment
Higher incidence of dysmorphisms (e.g., vacuoles, cytoplasmic granularity)
Altered genetic stability and metabolism
Interestingly, different stimulation drugs (GnRH agonists vs. antagonists, FSH vs. hMG) show mixed results in their effects on oocyte health. Some studies suggest antagonists improve quality and reduce aneuploidy risks, while others find no significant difference.
Impact on the Endometrium
Stimulation protocols don’t just affect the eggs – they also influence endometrial receptivity. In some cases, stimulation can cause the endometrium to mature prematurely, leading to lower chances of implantation. This has led to strategies like “freeze-all” cycles, where embryos are frozen and transferred later when the endometrium is more receptive.
The future of ovarian stimulation lies in individualization:
Using genetic markers (like LH receptor polymorphisms) to predict response.
Incorporating AI and deep learning for follicular growth tracking.
Tailoring stimulation doses to maximize safety while preserving quality.
Conclusion
Ovarian stimulation remains both an art and a science. As Dr. Rama Raju emphasized, success depends not only on retrieving more eggs but on ensuring the highest quality oocytes and a receptive uterine environment. Ongoing research, technology integration, and patient-specific approaches are paving the way for safer, more effective IVF treatments.
