Hysteroscopy Explained: A Minimally Invasive Solution for Women’s Health and Fertility
Category: Women’s Health / Fertility Treatment
Author: DR G A RAMARAJU
At Krishna IVF, we are committed to using the latest technology to provide precise diagnoses and effective treatments. Whether you are struggling with unexplained infertility or experiencing abnormal menstrual bleeding, getting a clear view of what is happening inside the uterus is often the key to finding a solution.
One of the most effective tools we use is Hysteroscopy.
If your doctor has recommended a hysteroscopy, you likely have questions. What is it? Is it painful? How will it help me? In this blog, we break down everything you need to know about this minimally invasive procedure.
What is Hysteroscopy?
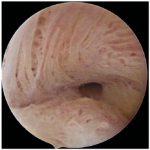
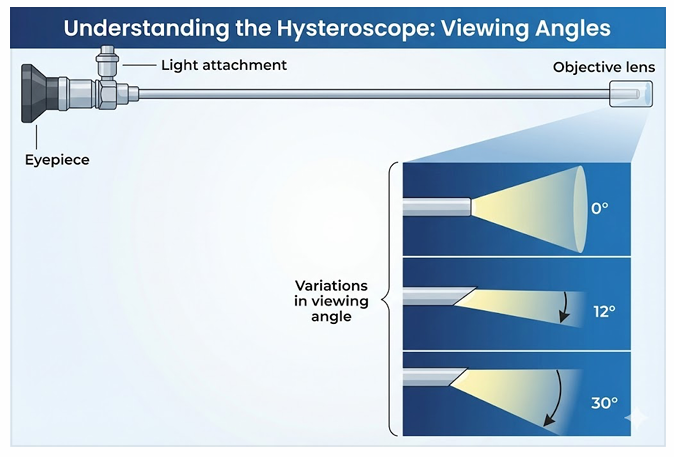
A hysteroscopy is a procedure that allows your doctor to look inside your uterus (womb) to diagnose and treat causes of abnormal bleeding or fertility issues. We use a hysteroscope-a thin, lighted telescope-like instrument. It is inserted through the vagina and cervix into the uterus. Because it enters through natural pathways, there are no cuts or incisions on your skin.
There are two main types of hysteroscopy, often performed together:
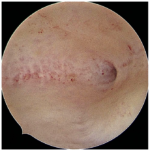
1. Diagnostic Hysteroscopy: Used to simply “look” and diagnose problems like polyps, fibroids, or structural issues.
2. Operative Hysteroscopy: If a problem is found during the diagnosis, we can often use specialized, slender instruments to correct the issue mmediately (e.g., removing a polyp).
Why is Hysteroscopy Performed?
Hysteroscopy is the “Gold Standard” for evaluating the uterine cavity. At Krishna IVF, we may recommend this procedure for:
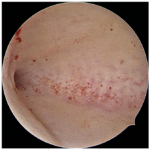
● Infertility Evaluation: To check for blockages, scar tissue, or uterine shapes (like a septum) that might prevent pregnancy.
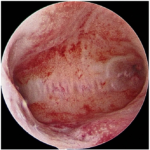
● Abnormal Uterine Bleeding: To investigate heavy periods, bleeding between periods, or post-menopausal bleeding.
● Polyps and Fibroids: To detect and remove non-cancerous growths inside the uterus.
● Recurrent Miscarriage: To identify if uterine abnormalities are causing pregnancy loss.
● Displaced IUDs: To locate and remove intrauterine devices that have moved out of place.
● Adhesions (Asherman’s Syndrome): To remove scar tissue inside the uterus that can cause absent periods and infertility.
The Benefits of Office Hysteroscopy
Thanks to advancements in technology, we now use smaller diameter hysteroscopes (some as thin as 3 to 5mm). This offers significant benefits to our patients:
● Minimally Invasive: It avoids the risks of major surgery.
● Accuracy: Unlike “blind” procedures like D&C (Dilation and Curettage), hysteroscopy allows us to see exactly where the problem is, ensuring we don’t miss focal pathology.
● Quick Recovery: Most patients go home the same day and resume normal activities within 24 hours.
● See and Treat: We can often diagnose and fix the problem in a single visit, streamlining your treatment plan.
What to Expect During the Procedure
Preparation: We generally schedule the procedure shortly after your period ends (the proliferative phase) when the view of the uterus is clearest. We may prescribe medication (like misoprostol) the night before to help soften the cervix, making the procedure easier and more comfortable.
During the Procedure:
1. You will be positioned comfortably, similar to a pap smear exam.
2. Depending on the complexity, we may use local anesthesia (to numb the cervix) or mild sedation to ensure you are comfortable. Many diagnostic procedures are virtually painless and require no anesthesia.
3. The hysteroscope is gently guided into the uterus.
4. We release a fluid (usually saline) to expand the uterus, giving us a clear view of the lining and the openings of the fallopian tubes.
5. If we find issues like polyps or adhesions, we can remove them using tiny instruments.
The procedure is usually quick, often taking less than 30 minutes.
Is Hysteroscopy Safe?
Yes, hysteroscopy is generally very safe. Serious complications are rare (occurring in less than 1% of cases).
However, as with any medical procedure, there are minor risks, which we will discuss with you. These can include infection or rarely, a small perforation of the uterine wall.
Note: Hysteroscopy is never performed if you are pregnant or have an active pelvic infection.
Recovery and Aftercare
Most women feel fine shortly after the procedure. You might experience:
● Mild cramping (similar to menstrual cramps).
● Light spotting or bleeding for a few days.
You can typically treat any discomfort with over-the-counter pain relievers like acetaminophen or ibuprofen. We recommend resting for the day, but you can usually return to work the next day.
The Bottom Line
Hysteroscopy has revolutionized how we treat gynecological and fertility problems. It eliminates the guesswork, allowing the team at Krishna IVF to see the problem clearly and treat it effectively-helping you get back to your life, or closer to your dream of starting a family.
Do you have concerns about heavy bleeding or fertility?
Contact Krishna IVF today to schedule a consultation and see if hysteroscopy is the right step for you.