Unlocking the Potential of the Junctional Zone: A New Frontier in Fertility Care
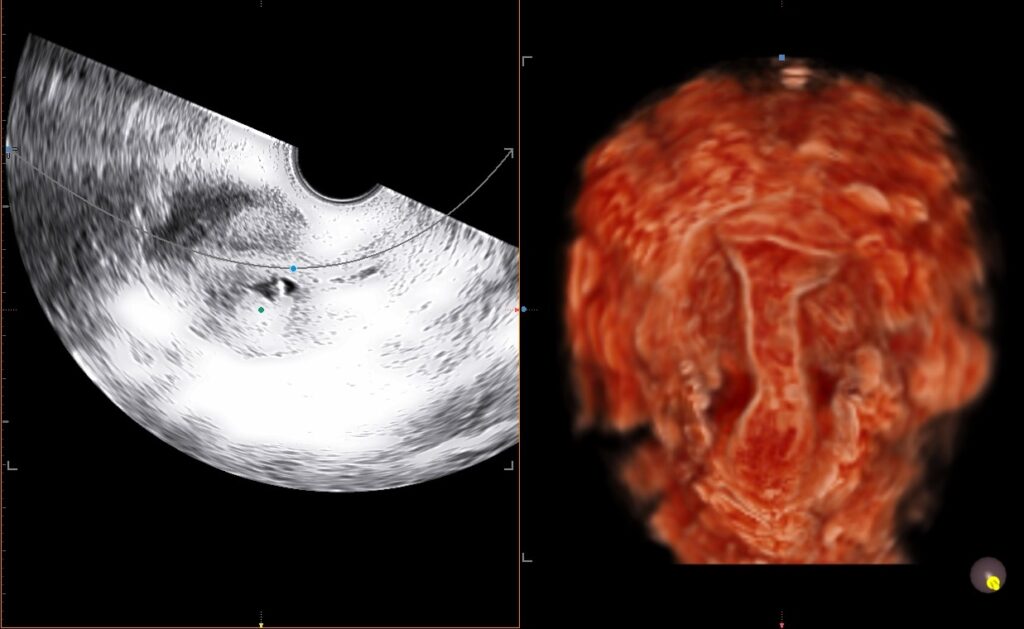
The uterus is a marvel of reproductive science, and its intricate layers work in harmony to support embryo implantation. Among these layers, the junctional zone (JZ) has recently emerged as a critical determinant of implantation success, reshaping the way clinicians approach fertility treatments. With advanced imaging technologies like 3D ultrasound and the power of artificial intelligence (AI), researchers are uncovering the pivotal role of the JZ in assisted reproduction, paving the way for more personalized and effective fertility care.
What is the Junctional Zone?
The junctional zone is a transitional layer located between the inner endometrium and the outer myometrium of the uterus. This specialized region has unique structural and functional characteristics that make it central to reproductive health. Subtle changes in the thickness, texture, and uniformity of the JZ have been linked to uterine receptivity, which is a key factor in successful embryo implantation. Yet, until recently, the JZ was often overlooked due to the limitations of conventional imaging techniques.
The Role of AI and 3D Ultrasound
In their groundbreaking study titled “Predicting Implantation Success Using Junctional Zone Assessment in Assisted Reproduction” (Ultrasound in Obstetrics & Gynecology, 2018), Dr. G.A. Ramaraju and his team at Krishna IVF harnessed the potential of 3D ultrasound combined with AI to evaluate the JZ with unprecedented precision.
3D Ultrasound: This advanced imaging modality provides detailed, high-resolution views of the uterus, allowing clinicians to visualize and measure the JZ in three dimensions. Unlike traditional 2D ultrasound, which can only offer limited insights, 3D ultrasound captures the complexity of the JZ’s structure and facilitates more accurate assessments.
AI Integration: By analyzing vast amounts of imaging data, AI algorithms identify patterns and anomalies in the JZ that might otherwise go unnoticed. This technology not only enhances diagnostic accuracy but also reduces variability in interpretations, ensuring consistent and reliable results.
Key Findings from the Research
Dr. Ramaraju’s study revealed several important insights:
Correlation with Implantation Success: The research demonstrated a strong association between JZ characteristics and the likelihood of successful implantation. Women with a thinner, more uniform JZ showed higher rates of implantation compared to those with irregular or thicker zones.
Personalized Treatment Planning: By assessing the JZ, clinicians can tailor fertility treatments to each patient’s unique uterine profile. For example, patients with suboptimal JZ conditions might benefit from targeted interventions to improve uterine receptivity before embryo transfer.
Empowering Patients and Clinicians: The integration of AI in JZ assessment provides patients with clear, evidence-based explanations of their fertility potential, fostering trust and informed decision-making.
Implications for Fertility Care
The implications of this research are profound. For patients, the ability to predict implantation success based on JZ assessment offers new hope and clarity in the often-uncertain journey of infertility treatment. For clinicians, it represents a significant advancement in personalized medicine, enabling them to deliver care that is both precise and effective.
Moreover, this approach underscores the importance of holistic uterine health in fertility outcomes. While factors like egg quality and embryo viability have traditionally taken center stage, the uterus itself is now receiving the attention it deserves as a critical component of reproductive success.
Looking Ahead: The Future of Fertility Treatment
The fusion of cutting-edge technologies like 3D ultrasound and AI with clinical expertise is transforming the landscape of reproductive medicine. As research into the JZ and other uterine factors continues to evolve, we can expect even greater strides in understanding and enhancing uterine receptivity.
At Krishna IVF, we remain committed to advancing the science of fertility care. By staying at the forefront of research and innovation, we aim to empower individuals and couples with the knowledge and tools they need to achieve their dreams of parenthood.
Conclusion
The junctional zone may be a small and often-overlooked part of the uterus, but its impact on implantation success is monumental. Thanks to the pioneering work of researchers like Dr. Ramaraju, we are beginning to unlock the secrets of this remarkable region, offering new pathways to hope and healing for families worldwide.
For more information on this research and how it could benefit you, visit https://krishnaivf.com/contact-us/. Let’s continue the conversation and explore how science and compassion can work together to create miracles.
