Karyotyping Genetic Test
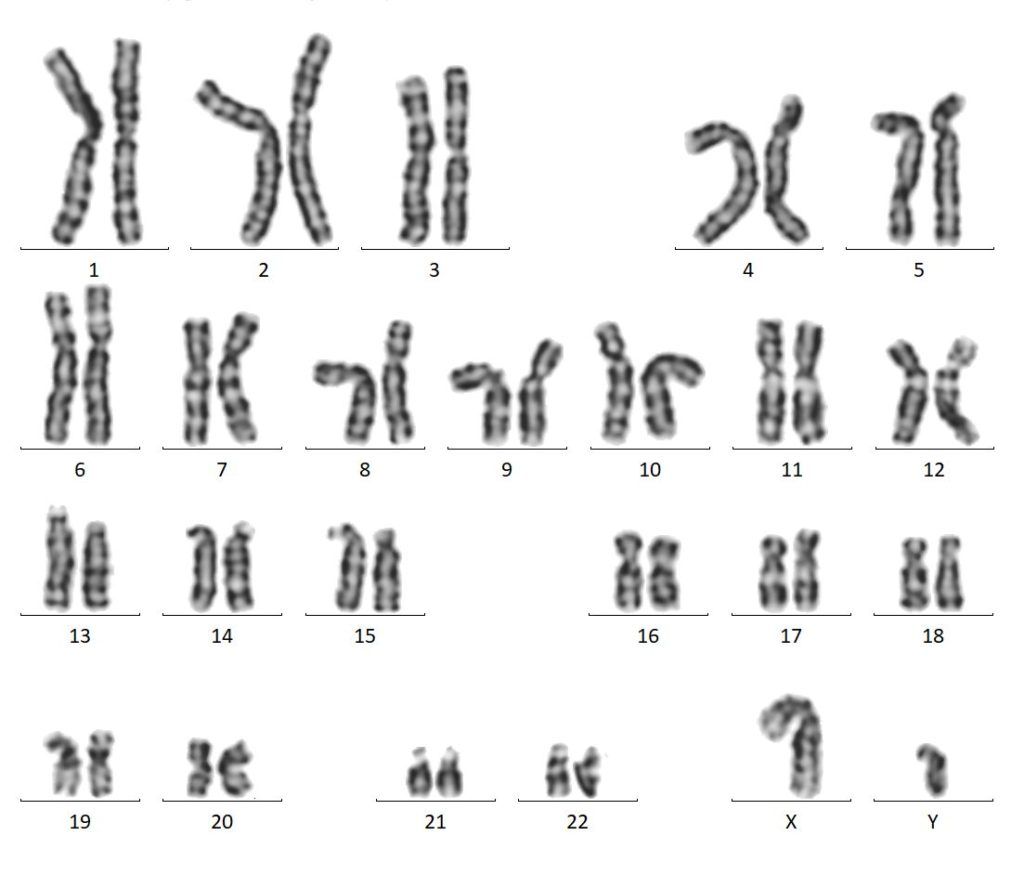
The Karyotype is the image of the chromosomes of an individual. Cytogeneticists prepare a complete set of metaphase chromosomes from each cell of an individual organism. Different types of specimens can be used like peripheral blood, CVS, amniotic fluid, bone marrow aspirations, and tissue. Cytogenticist takes a photograph of metaphase chromosome from a cultured specimen of an individual and arranges the chromosomes according to their size, centromeric position, and banding pattern. Karyotype describes the number of chromosomes and any structural abnormality. Humans contain 23 pairs of chromosomes.
Chromosomes were first discovered by swiss botanist Karl Nageli in pollen in the year 1842. Since its discovery, different scientists used improved methods to prepare metaphase chromosomes and different staining techniques to study 23 pairs of human chromosomes. In 1956 Joe HinTijo and Albert Levan developed an improved methodology to arrest the cells at metaphase using colchicine and used hypotonic solution to prepare better chromosome spread. In 1970, scientists developed different banding techniques like C, Q, and G to reveal complex structural abnormalities.
The bands on individual chromosomes are specific and are representations for euchromatin (light band)and heterochromatin (dark band)regions.The euchromatin region is less condensed and transcriptionally active where as heterochromatin is highly condensed and transcriptionally inactive.The regions have been identified using a variety of banding techniques and are numbered according to the landmark system adopted at the Paris Conference (1971). The landmarks and band numbers have been selected to make comparisons with the human karyotype simpler, and chromosomes have been arranged homologies with the specific human chromosomes.The International System for Human Cytogenetic Nomenclature is the standard tool to describe the human chromosomes and chromosomal aberrations (ISCN) which was established in 1978. Based on the location of centromere (Meta , sub meta & acrocentric)and the size, Human chromosomes can be classified into 7 gropus from A to G. A-group consists 1,2 &3 ;B –group consists 4& 5 ; C-group consists 6 to 12 & X ; D-group consists 13-15; E-group consists 16-18; F-group consists 19 & 20; G-group consists 21, 22 & Y chromosomes respectively.
Chromosomal Banding Techniques:
a) Those resulting in bands distributed along the length of the whole chromosome e.g.; G, Q & R
b) Those that stains a restricted number of specific bands or structures e.g.; C & NOR
Type A:
- G banding: The cultured metaphase chromosomes are treated with acid and proteolytic enzymes and stained with giemsa.The darkly stained regions contain AT rich nucleotides and lightly stained regions contain GC nucleotides.
- Q banding: This technique usesquanicrine mustard a fluorescent dye which produces specific type of banding pattern for each human chromosome, which gives alternate bright and dull bands represents hetero and euchromatin regions. This helps to identify variability in size and intensity of certain regions on the chromosomes.
- R banding: This technique helps to identifying abnormalities involving the terminal regions of the chromosomes, which are lighter stained by G- or Q- banding. This is attained by treatment of chromosomes in salineat high temperatures followed by giemsa staining.
Type B:
- C banding: This technique helps to identify heterochromatin around the centromere. This is attained by treating chromosomes with HCl, barium hydroxide and 2X SSC followed by giemsa stain.
- AgNOR banding: NOR banding is useful to identify specific chromosomal regions that form and maintain the nucleoli located on the stalks of acrocentric chromosomes. This is attained by treating with gelatin and sliver nitrate solution.
Chromosomal abnormalities:
Offsprings inherit 23 chromosomes from their mother and 23 from their father. Inspite of the high regulatory process of cell division, sometimes offsprings inherit abnormal chromosomes either a numerical change or a structural change. Karyotype test helps to identify these abnormalities in the offspring.This test helps to identify abnormal babies during certain weeks of pregnancy and helps to avoid giving birth to genetically compromised offspring.
Chromosomal abnormalities are of two types:
a) Numerical abnormalities includes:
Numerical abnormality is the variation in number of particular chromosome within the pair of chromosomes.
Eg;.,Down’s Syndrome (Trisomy 21), Edward’s Syndrome (Trisomy 18), Patau’s syndrome (Trisomy 13), Klinefelter’s syndrome (47, XXY), Turner’s syndrome (45 X0), Jacob’s syndrome (47XYY).
b) Structural abnormalities include:
- Deletion: portion of chromosome is deleted and chromosomal deficiency occurs either terminally or interstitial eg; Cri du chat syndrome(5p-), Di George syndrome(22q11.2), Angelman syndrome ( 15q11.2-q13).
- Duplication: part of the chromosome is duplicated and is usually caused by abnormal events of recombination and tend to be less detrimental (Pallister-Killian syndrome, where part of the #12 chromosome is duplicated).
- Inversions: It is a type of chromosomal rearrangement and the segment is inverted or flipped either in one arm (paracentric) or in two arms around the centromere (pericentric).e.g.; 9 (inv[9][p11q13])
- Translocations occurs when a part or segment of one chromosome breaks and becomes attached to other chromosome. Translocation occurs between two non-homologous chromosomes (reciprocal) t(8;14) translocation in Burkitt’s lymphoma) and between two acrocentric chromosomes (Robertsonian ){45,XY, rob(13;14)}.
- Isochromosome or ring chromosome forms when breaks occur in both arms of a chromosome and broken ends anneal to form a ring chromosome.
- The polymorphic variants are most commonly present on non-acrocentric chromosome in the pericentric heterochromatin on long arms (q) of 1, 9 and 16 (1qh+/−, 9qh+/-, inv (9),16qh+/−), and short arms (p) of acrocentric chromosomes(13p+,14p+,15p+) and distal heterochromatin of Y chromosome (Yqh+/−).
When to do?
- During certain weeks of your pregnancy, your doctor will suggest which karyotype test is right for you based on how far along you are in your pregnancy and on your risks.
- It’s more likely your baby could have a chromosome problem if:
- You’re 35 or older.
- You have another child or a family member who has a chromosome disorder.
- You or your partner has something unusual in your chromosomes.
- You have a history of miscarriages or had a baby that was stillborn.
- Parental karyotype is suggested if the fetus with chromosomal abnormality, miscarriage with suspected chromosomal abnormality, multiple miscarriages or neonatal deaths is identified.It is done on venous blood collected from both the parents.
Fetal Karyotyping: Cytogenetic analysis of fetal cells conventionally requires amniotic fluid, chorionic villi, or fetal blood, which are sampled through amniocentesis, chorionic villus sampling (CVS), and cordocentesis, respectively.The sample collection procedures are invasive and have a risk of miscarriage.
Amniocentesis is usually performed between 16 and 28 weeks of gestation. A needle is used to aspirate approximately 20 mL of amniotic fluid under the guidance of ultrasound imaging. The risk of abortion is 1% but increases considerably if performed prior to 15 weeks of gestation.
CVS sampling from the developing placenta is usually performed between 10 and 12 weeks of gestation. Tissue samples are collected using a catheter attached to a syringe under the guidance of real-time ultrasonograms. One advantage of CVS is that it enables an early and definitive chromosomal analysis. CVS have a greater risk of fetal loss.
Cordocentesis sampling of fetal blood from the umbilical vein is usually performed between 16 and 37 weeks of gestation. A spinal needle is inserted near the placental origin of the umbilical vein, and blood is drawn under the guidance of ultrasound. Kleihauer testing is performed to confirm the absence of maternal blood contamination. It has a decreased risk for miscarriage.
Karyotype on product of conception (POC) which is fetal tissue from a miscarriage to determine if the lost pregnancy was the result of a chromosomal abnormality. This test can provide you important information about the possible causes of your patient’s miscarriage to help them to plan future pregnancy.